An international study led by CIC bioGUNE provides new advances in the study of the progression of metabolic liver disease

Metabolic liver disease (MetHD), the most common with a global prevalence of 30%, can progress to steatohepatitis (MASH), characterised by fat accumulation and liver inflammation, increasing the risk of fibrosis, cirrhosis and liver cancer.
A new study, published in the journal Metabolism, provides further evidence on the mechanisms regulating the liver enzyme glutaminase 1 (GLS) in metabolic liver disease, highlighting its role in the ammonium accumulation in the liver that is characteristic of steatohepatitis.
A study published in the journal Metabolism has revealed potential mechanisms underlying the regulation of the liver enzyme glutaminase 1 (GLS) in metabolic liver disease (MetHD) and highlighted the important role of GLS in the accumulation of ammonium in the liver, a hallmark of steatohepatitis.
The international study has been led by Dr Malu Martínez-Chantar, leader of the Liver Diseases Laboratory Group at CIC bioGUNE – a member of BRTA – and CIBEREHD and the “Ramón y Cajal” and Ikerbasque researcher Teresa Cardoso Delgado from the Biobizkaia Health Research Institute (IIS Biobizkaia) and has involved colleagues from CIMUS, ISPA, CINN, IUOPA, UPV/EHU and UCL in the UK.
Metabolic liver disease (MetHD), formerly known as non-alcoholic fatty liver disease (NAFLD), is the most common type of chronic liver disease worldwide, with a global prevalence of 30%. Steatohepatitis (MASH) is a progressive form of EHmet, characterised by a marked accumulation of fat in liver cells (steatosis), dead liver cells (“balooining” and degeneration) and liver inflammation. Patients with MASH are at increased risk of liver-related morbidity and mortality and metabolic comorbidities, such as liver fibrosis, cirrhosis, liver cancer and cardiovascular disease. Understanding the mechanisms and causes underlying the progression from simple steatosis to MASH is important to recognise at-risk patients and potential therapeutic targets.
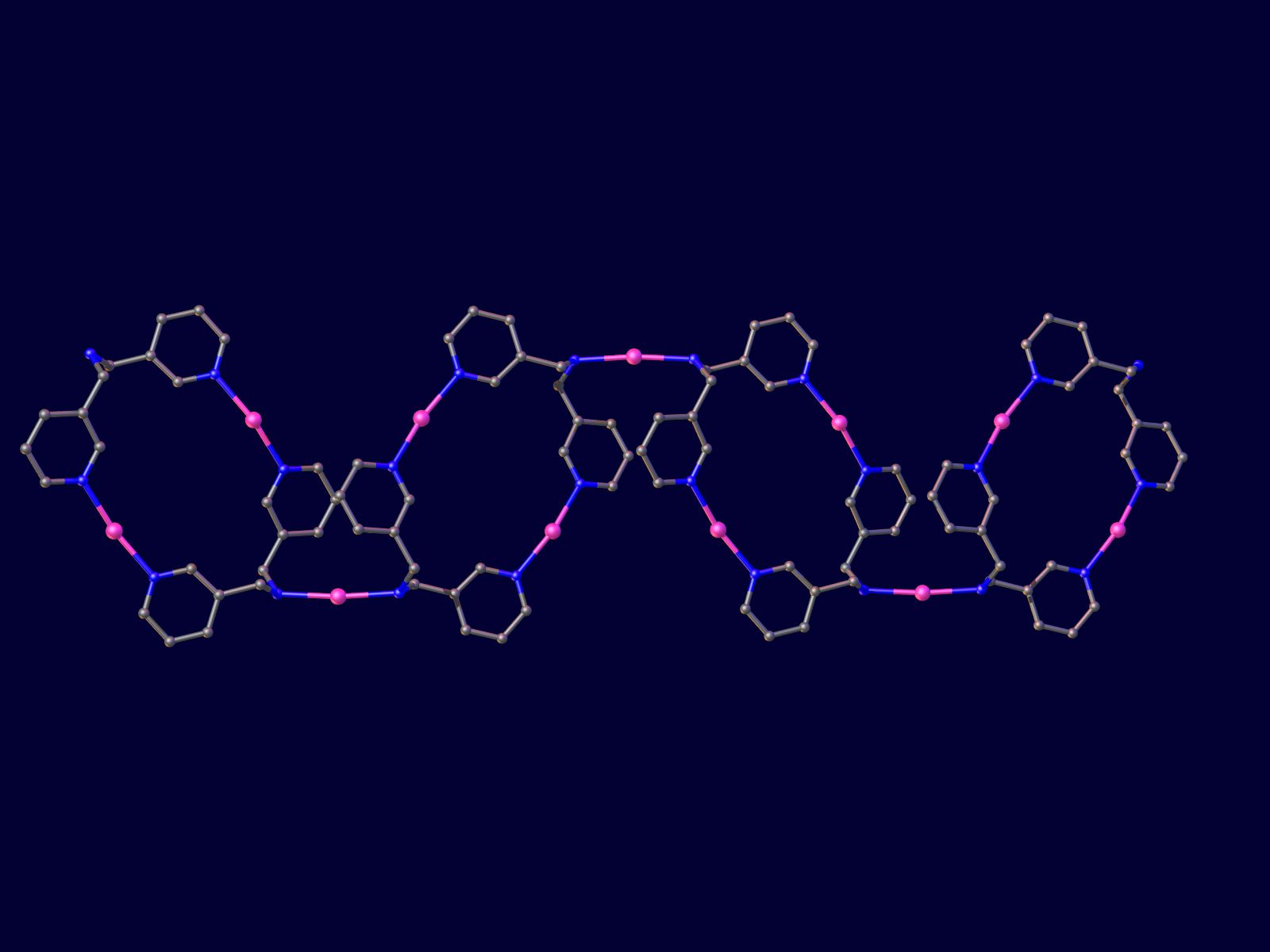
In this study by Maria Mercado-Gomez et al, the authors have shown that the enzyme glutaminase 1 (GLS), which converts glutamine to glutamate and the toxic by-product ammonium, is a hallmark of MASH in liver biopsies from preclinical models and HDmet patients. Ammonium has been suggested as a pathogenic factor potentially responsible for MetH disease-related multi-organ dysfunction and disease progression. Importantly, downregulation of hepatic GLS in preclinical models of EHmet is sufficient to reduce hepatic ammonium, suggesting an important role for this enzyme in the pathogenic accumulation of hepatic ammonium underlying EHmet.
In addition, the authors have described that lipopolysaccharide (LPS), large molecules found in the membrane of some types of bacteria, can increase GLS expression in the liver, while pharmacological inhibition of the LPS receptor, Toll-like receptor 4 (TLR4), hinders GLS upregulation. Overall, these results are consistent with a large body of literature indicating that gut microbiota and bacterial products can directly and indirectly affect the liver through a variety of mechanisms, leading to a wide range of liver diseases, including EHmet.
The financial support provided by the Ministry of Science, Innovation and Universities of the Government of Spain (AEI), the Ikerbasque Foundation, the La Caixa Foundation, the Carlos III Institute of Health, the Basque Government Departments of Education, the Gilead Sciences International Research Fellows Programme and CIBERehd has been fundamental for the realisation of this project.