New study reveals how genetic defects in carbohydrate digestion influence dietary response in irritable bowel syndrome patients

Irritable bowel syndrome (IBS) affects up to 10% of the world’s population and remains difficult to treat due to the wide variability in patients’ symptoms and their responses to dietary or pharmacological interventions.
An international study, published in Clinical Gastroenterology & Hepatology, shows increased efficacy of dietary interventions in IBS patients with genetic defects in carbohydrate digestion.
This research could lead to personalised treatments for IBS, using genetic markers to predict which patients will benefit from specific dietary interventions.
Research from CIC bioGUNE and LUM University (Italy), published today in Clinical Grastroenterology & Hepatology, has revealed that genetic defects in carbohydrate digestion influence the dietary response of patients with irritable bowel syndrome (IBS). The work opens the door to personalised treatments for IBS, using genetic markers to predict which patients will benefit from specific dietary interventions.
IBS is a digestive disorder that affects up to 10% of the world’s population and is characterised by abdominal pain, bloating, diarrhoea or constipation. Despite its prevalence, treatment of IBS remains a challenge, as symptoms and responses to dietary or pharmacological interventions vary significantly. Patients often associate their symptoms with the consumption of certain foods, especially carbohydrates, and the elimination or reduction of these in the diet has emerged as an effective treatment option, although not all patients experience the same benefits.
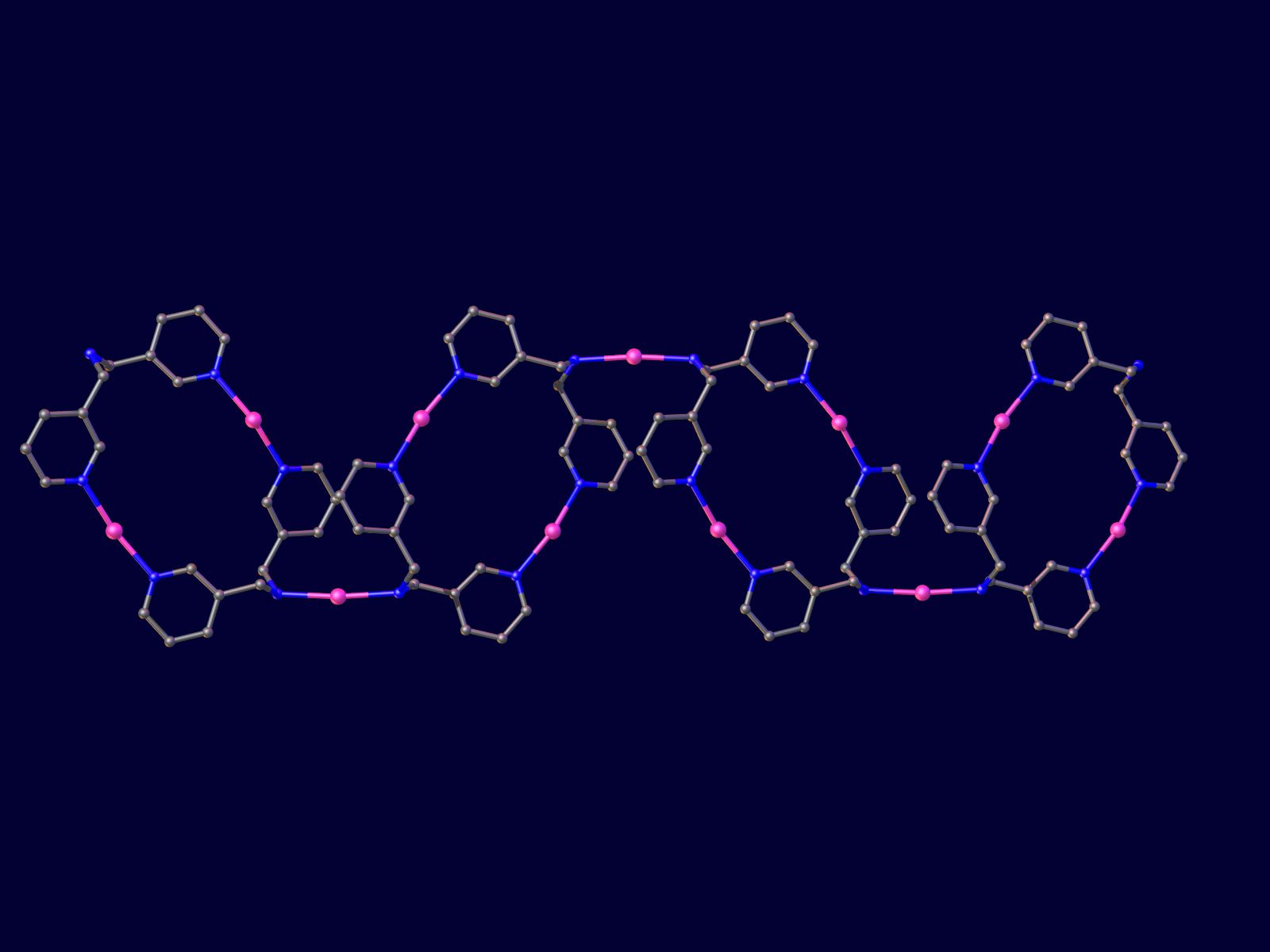
Nutrigenetics (the science that investigates the combined action of our genes and nutrition on human health) has highlighted how changes in DNA can affect the way we process food. One well-known example is lactose intolerance, where loss of lactase enzyme function makes it difficult to digest dairy products. Now, a pioneering study published in the journal Clinical Gastroenterology & Hepatology suggests that genetic variations in human carbohydrate-active enzymes (hCAZymes) may similarly affect how IBS patients respond to a reduced carbohydrate (low FODMAP) diet.
The research, led by Ikerbasque Research Professor Mauro D’Amato from the Gastrointestinal Genetics Group at CIC bioGUNE – a BRTA member – and the Department of Medicine and Surgery at LUM University, has investigated the role of hCAZymes in relation to IBS. Through a large international collaboration (the GenMalCarb consortium) and data from the DOMINO trial, the team revealed that individuals with hypomorphic (defective) variants in the hCAZymes genes are more likely to benefit from a reduced carbohydrate diet. The study, which involved 250 IBS patients, compared two treatments: a diet low in fermentable carbohydrates (FODMAP) and the antispasmodic drug otilonium bromide. Surprisingly, of the 196 patients on the diet, those carrying defective hCAZyme genes showed a marked improvement compared to non-carriers, and the effect was particularly pronounced in patients with diarrhoea-predominant IBS (IBS-D), who were six times more likely to respond to the diet. In contrast, this difference was not observed in patients who received medication, underscoring the specificity of genetic predisposition in the efficacy of dietary treatment.
‘These findings suggest that genetic variations in hCAZyme enzymes, which play a key role in carbohydrate digestion, could become critical markers for designing personalised dietary treatments for IBS,’ says Mauro D’Amato, lead author of the study. ‘The ability to predict which patients respond best to a reduced carbohydrate diet has the potential to strongly impact the management of IBS, improving adherence and outcome.
In the future, incorporating knowledge of hCAZymes genotype into clinical practice could allow clinicians to identify in advance which patients are most likely to benefit from specific dietary interventions. This would not only avoid unnecessary restrictive diets for those who are unlikely to benefit, but would also open the door to personalised medicine in IBS. The research team emphasises the need for further studies to validate these findings and delve deeper into the biological mechanisms at play. If confirmed, this approach could dramatically improve the treatment of IBS and similar gastrointestinal conditions, making dietary and therapeutic strategies more precise and effective.